While perhaps not a favorite subject, and not a favorite appointment for many patients, is a women’s health screening exam. Although widely regarded as a necessary but unpleasant life experience, the Papanicolaou test (or Pap) and regular annual checkups have demonstrated effectiveness in dramatically reducing rates of cervical cancer, a potentially fatal disease process.
Fortunately many advancements in medical science have greatly improved early detection, and even prevention of this deadly disease. As January is cervical health awareness month, this may be a great time to review some of the recent changes in recommendations and practices. Many of us trained and grew up in an era where there was increased awareness and screening for cervical cancer, but not much to be done about it other than early detection, surveillance and surgery.
As such, it was recommended for most women to have Pap screening early and often – either three years after first intercourse, or at 18 years of age. After that, annually until a cutoff age was typical. The Pap smear to identify cells with concerning features is still an integral part of women’s health, although age recommendations have changed dramatically.
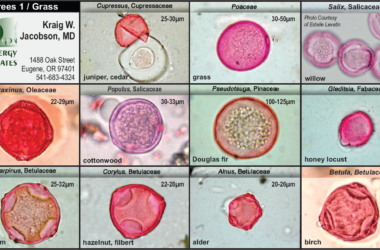
One of the most important changes in screening for cervical cancer has been the development of the human papilloma virus (HPV) co- test, which is the ability to check for the presence of high risk strains of HPV along with traditional Pap testing. HPV is a family of viruses that include viruses responsible for warts, but also includes viruses that can cause a silent or nearly silent infection of the skin, vagina or cervix that results in changes in the cells predisposing them to malignancy.
Scientists have determined that while many screenings may be positive for a number of reasons, including benign changes in the cervix, presence of high-risk strains of HPV were often the deciding risk factor that predispose patients to the development of cervical cancer (and rarely, penile cancer in men). As a result, it was possible to further target screenings and decrease the frequency of screenings of the general population. Information about additional strains of HPV is constantly being discovered, and these changes update recommendations for screening regularly.
In addition to increased sensitivity and specificity of screening practices, another exciting new development has been the HPV vaccine that is now available. Initially released protecting against four different high-risk strains of HPV, a newer vaccine is now available that protects against a total of nine high- risk strains.
It is very effective and remains one of the only vaccines available that can prevent cancer. Even if a patient has been exposed to one or more strains, the vaccine will still protect against additional strains in future exposures. It may also protect against reactivation as the HPV virus can often lay dormant for many years before causing any symptoms.
Initially target audiences included young women, but in 2018 guidelines were liberalized to recommend vaccination for men and women, boys and girls aged nine through 44. This was a major change, previously targeting age groups nine through 26. The vaccine consists of a three-shot series for patients over 15 years of age, and a two-shot series for those 15 and under.
The result of these improvements in the care and evaluation of women’s health are recommendations for cervical cancer screenings with Pap testing not to be initiated until 21 years of age, and every three years until age 29, followed by screening every five years with HPV testing until age 65, regardless of vaccination status.
This dramatically decreases the frequency of screening required, and accordingly decreases the risk of false positive tests that may require additional invasive procedures. It is important to note that for patient’s health still benefits from seeing a doctor once a year for an annual checkup, and reporting any changes in your health along with a thorough physical examination.
The change is that for most women, with otherwise normal previous screening, it means much less anxiety about an annual checkup; along with more confidence in medicine’s ability to detect and address cervical cancer before it ever has a chance to get started.
Camas Swale Medical Clinic provides full spectrum family care including Women’s Health, family planning and contraception management. The HPV vaccine is available at primary care clinics and select pharmacies.